A new study just out reveals that HIV takes hold in the human body with the help of cells that usually work to heal, not kill.
HIV invades the body through genital or rectal mucous membranes. Exactly how that occurs on a molecular level was not understood until now. The study reports a common mucosal cell may be responsible for increasing the ability of HIV to infect human immune cells.
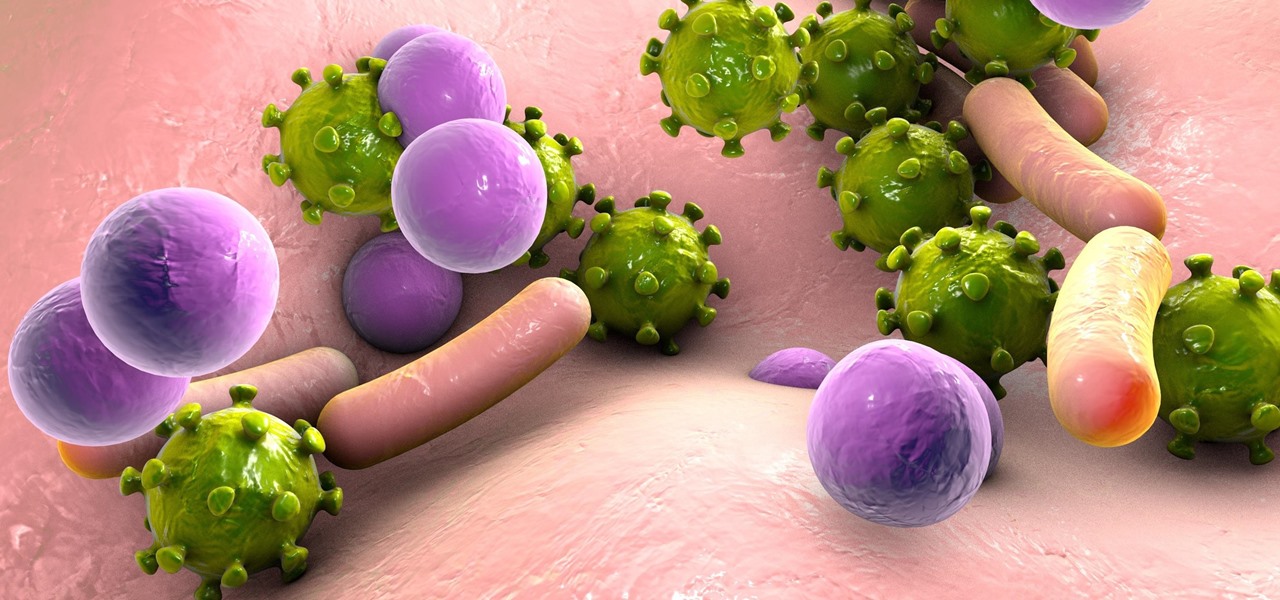
Human immunodeficiency virus (HIV) targets CD4 cells called T cells. Because these cells are critical to immune function, their loss from attack by HIV leaves the body unable to fight off infection, resulting in development of acquired immunodeficiency syndrome (AIDS).
At present, there is no cure for HIV, but drug therapies enable many HIV-positive patients to enjoy full lives. According to the Centers for Disease Control and Prevention, there are more than 12 million people in the US with HIV, and approximately one in eight individuals are unaware they are infected.
In the collaborative study, published in PLOS Pathogens from researchers at the Gladstone Institutes and the University of California, San Francisco (UCSF), as well as from European collaborators, it was found that abrasions in the mucosal lining give HIV access to cells that enhance its ability to infect T cells.
A Killer Disease Gets Help from Human Cells
To stop transmission of HIV, we have to know how it infects humans. This study takes an important step closer to understanding where to intervene in that process to reduce or eliminate the ability of HIV to infect immune cells.
The research team wanted to know more about how HIV maneuvers past the cells of the mucous lining of the body that are intended to protect against invasive pathogens.
The skin is the first line of defense against infectious germs. Pathogens also approach the body through the respiratory system, eyes, genitals, and rectum. These gateways, and all internal organs in the body, are lined with mucous membrane composed of epithelial tissue, which are tightly woven sheets of cells with functions that include defense against infectious disease.
Among the cells of the epithelial layer are dendritic cells. These cells are responsible for signaling and mounting an immune response to invading pathogens.
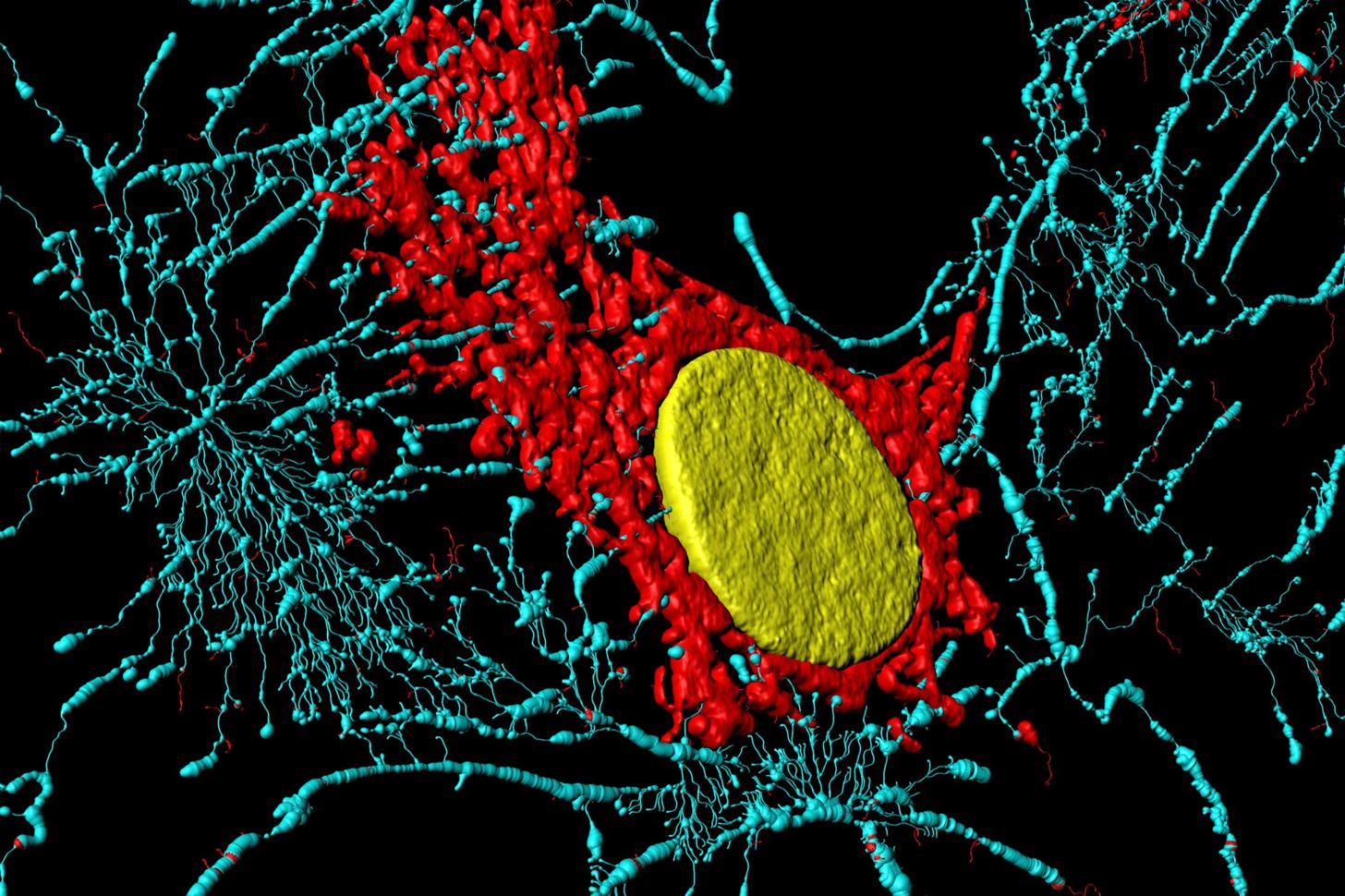
Lying within the epithelial tissue are cells called fibroblasts, spindle-shaped cells that synthesize collagen and create connective tissue. As a group, stromal cells like fibroblasts are part of the nutritional matrix that connects and gives form to the body and its organs.
In this study, researchers found that fibroblasts in the mucous membrane of the foreskin, male urethra, intestines, uterus, and cervix actually increase the ability of HIV to cross the mucous membrane and invade T-cells.
The study suggests that fibroblasts, one of the most common and abundant cells in the body, routinely move HIV through mucosal tissue without being infected. Study authors report fibroblasts increase the possibility of infection by certain strains of HIV by "up to 100-fold." This process, by which cells carry infectious microbes to another cellular target, is known as "trans-infection."
Dendritic cells, themselves resistant to HIV, also carry the infectious microbe to T-cells, but appear to be less effective given their lower numbers and relative inefficiency in transferring the virus. Unlike fibroblasts, dendritic cells are capable of initiating an immune response to the HIV, making fibroblasts a safer target for the virus.
By itself the epithelial layer in the mucous membrane emits an antiviral substance to kill passing pathogens. But when the epithelial layer is breached, HIV has access to fibroblasts that carry it into the body.
Surprisingly, the exchange of fluids during sex by itself does not efficiently transmit HIV. Instead, it is tiny tears or abrasions that occur during sex, or genital or rectal ulcers already present, that offer HIV an opening into the fibroblast-rich mucous membrane.
"We discovered that, remarkably, mucosal fibroblasts could potently increase how well HIV infected immune cells," Nadia Roan, a professor of urology at UCSF working at the Gladstone Institute, said in a press release. "Knowing how this occurs at the molecular level can help us find new ways to fight the virus."
The study used donated endometrial and cervical tissues from healthy women ages 18 to 49 years of age who were not pregnant and who were undergoing gynecologic procedures unrelated to infectious disease. Samples of foreskin, urethral, tonsil, and intestinal tissues were also obtained with consent. The tissues were separated, preserved, conditioned, cultured, and observed to investigate how the tissues behave with HIV to increase or reduce odds of infection.
"Knowing the specific cells that allow HIV to take advantage of breaches in our defenses will enable us to find better ways to limit HIV transmission rates." said Dr. Warner Greene, the director and senior investigator of the Virology and Immunology department at Gladstone," in the press release.
While the study identified fibroblasts as an agent in the trans-infection of HIV, fibroblasts and dendritic cells are also suspected to carry as-yet-unknown capabilities to "trans-enhance" the infection. Further studies are needed to understand how these epithelial cells could be improving environmental conditions for invasion by HIV.
Just updated your iPhone? You'll find new emoji, enhanced security, podcast transcripts, Apple Cash virtual numbers, and other useful features. There are even new additions hidden within Safari. Find out what's new and changed on your iPhone with the iOS 17.4 update.
























Be the First to Comment
Share Your Thoughts